Sabrina Pia Law, MD

Overview
Dr. Sabrina Law joined the Division of Pediatric Cardiology in 2014, and serves as medical director of the Pediatric Ventricular Assist Device (VAD) Program. During her tenure, NewYork-Presbyterian Morgan Stanley Children's Hospital has quintipled the number of VADs used as a bridge to transplantation or recovery. An integral member of the Program for Pediatric Cardiomyopathy, Heart Failure and Transplantation, she specializes in caring for children with end-stage heart failure secondary to congenital or acquired cardiomyopathies, failed palliated or non-palliated terminal congenital heart disease, and acquired cardiac disorders. Her clinical and research interests are focused on evaluating the use of ventricular assist devices for children with acute decompensated heart failure. She is the site co-principal investigator in a national trial evaluating the use of newer ventricular assist devices in small children (Pumps in kids infants and neonates - PumpKIN). Following completion of an advanced fellowship in Pediatric Heart Failure Cardiomyopathy and Transplantation at Texas Children’s Hospital, Dr. Law previously worked at Seattle Children’s Hospital, where she helped build the pediatric VAD program.
Areas of Expertise / Conditions Treated
- Cardiomyopathy
- Heart Transplant, Pediatric
- Pediatric Congenital Heart Disease
- Pediatric Heart Failure
- Ventricular Assist Device
Academic Appointments
- Associate Professor of Pediatrics at CUMC
Administrative Titles
- Medical Director, Pediatric Ventricular Assist Device Program
Hospital Affiliations
- NewYork-Presbyterian / Columbia University Irving Medical Center
- NewYork-Presbyterian Morgan Stanley Children's Hospital
Gender
- Female
Schedule an Appointment
Phone Appointments
Connect Patient Portal
For existing patients, login to make an appointment, view documentation or contact your care provider.
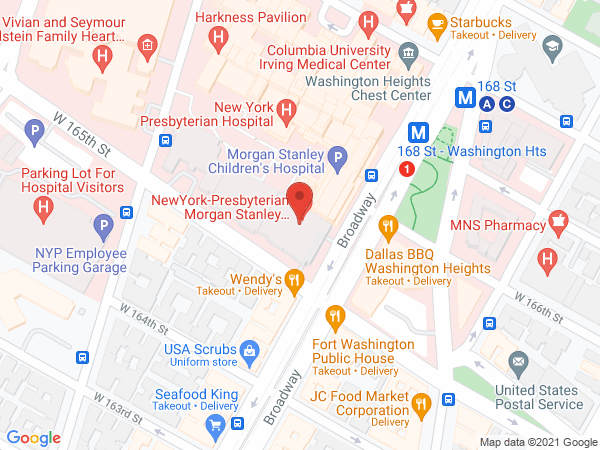
Location(s)
Insurance Accepted
Aetna
- Aetna Signature Administrators
- EPO
- HMO
- Medicare Managed Care
- NYP Employee Plan
- NY Signature
- POS
- PPO
- Student Health
Affinity Health Plan
- Essential Plan
- Medicaid Managed Care
Amida Care
- Special Needs
Cigna
- EPO
- Great West (National)
- HMO
- Medicare Managed Care
- POS
- PPO
Emblem/GHI
- Medicare Managed Care
- PPO
Emblem/HIP
- ConnectiCare
- EPO
- Essential Plan
- HMO
- Medicaid Managed Care
- Medicare Managed Care
- POS
- PPO
- Select Care (Exchange)
- Vytra
Empire Blue Cross/Blue Shield
- EPO
- HMO
- Medicare Managed Care
- PPO
Empire Blue Cross Blue Shield HealthPlus
- Child/Family Health Plus
- Essential Plan
- Medicaid Managed Care
Fidelis Care
- Child/Family Health Plus
- Essential Plan
- Medicaid Managed Care
- Medicare Managed Care
Healthfirst
- Child/Family Health Plus
- Leaf (Exchange)
- Medicaid Managed Care
- Medicare Managed Care
Local 1199
- Local 1199
MagnaCare (National)
- MagnaCare
Medicare
- Railroad
- Traditional Medicare
Multiplan
- Multiplan
MVP Health Care
- Child/Family Health Plus
- Essential Plan
- HMO
- Medicaid Managed Care
Quality Health Management
- Quality Health Management
UnitedHealthcare
- Compass (Exchange)
- Empire Plan
- HMO
- Medicaid (Community Plan)
- Medicare Managed Care
- Oxford Freedom
- Oxford HMO
- Oxford Liberty
- POS
- PPO
VNSNY CHOICE
- Medicare Managed Care
- SelectHealth
- Special Needs
WellCare
- Medicaid Managed Care
- Medicare Managed Care
World Trade Center Health Plan
- World Trade Center Health Plan
Credentials & Experience
Education & Training
- MD, 2002 St Johns National Academy of Health Sciences, India
- Residency: Westchester Medical Center - Maria Fareri Children's Hospital
Committees, Societies, Councils
- Advanced Cardiac Therapies Improving Outcomes Network (ACTION), Site PI. The ACTION learning network consists of clinicians, researchers, parents, and patients from across a 41 national and 5 international medical institutions. The goal is to improve critical outcomes for children with heart failure by uniting providers and families, sharing data and outcomes transparently, improving education and standardizing best practices. The current focus is on improving outcomes for pediatric ventricular assist device (VAD) patients. This VAD learning network approach allows us to make improvements faster across this collaborative system by the creation of clinical guidelines. The Harmonization, Patient Reported Outcomes and Global Quality Initiative committees meet once each per month per month by phone. An annual live meeting is held in addition to live half day or day long sessions at national meetings.
- Lead of Pediatric VAD Steering Committee. The goal of the committee is to provide input on the strategic planning and coordination of the Pediatric VAD Program. The committee seeks input from each discipline (Heart Failure/ Transplant, Perfusion, ICU, Floor and ICU Nursing Leadership, Floor and ICU nurses, Hematology as well as CT Surgery) to discuss how to best approach the different aspects of care for patients supported by VAD. Every discipline’s expertise is taken into consideration while incorporating policies, procedures, and education. So far the committee has been instrumental in developing institutional anticoagulation guidelines for ventricular assist devices in children, and instructional material and curriculum design used locally, as well as quality improvement protocols for the Transplant, Cardiomyopathy and Ventricular Assist Device Program
- Site PI and co-investigator for "Safety and Benefit of a Novel Anticoagulation Protocol for Berlin EXCOR." This prospective multicenter study is evaluating the adherence to, safety, and efficacy of a novel anticoagulation protocol for children supported on the Berlin Heart EXCOR. US Food and Drug Administration, Orphan products grant.
- Cardiology co-principal investigator for PUMPKIN Trial clinical site, NewYork-Presbyterian Morgan Stanley Children’s Hospital, New York, NY. PUMPKIN is a randomized, multicenter trial evaluating the investigational infant Jarvik 2000 Heart System versus the EXCOR pediatric device in pediatric patients with heart failure.
- Co-Chair for Task Force 9 titled “Pediatric VAD Program Development.” An International Society for Heart and Lung Transplant (ISHLT) Consensus Document titled “ISHLT Consensus Statement on Management of Pediatric and Congenital Heart Disease Patients with Ventricular Assist Devices.” The aim of this document is to provide recommendations that will assist programs in constructing selection and management protocols that can be efficiently administered
- Executive board member of the International Society for Pediatric Mechanical Cardiopulmonary Support (ISPMCS). The society brings together clinicians, bioengineers, and basic scientists to precisely define problems and suggest solutions with novel approaches.
Board Certifications
- Pediatric Cardiology
- Pediatrics
Honors & Awards
2019 Columbia University Irving Medical Center Leadership and Management Course for Faculty Designed for 28 CUIMC faculty annually who currently have leadership/management responsibilities under the leadership of the Columbia Business School, this program helps participants develop the knowledge and skills necessary for current and future leadership positions in the academic health sciences program offered by the Office of Faculty Professional Development, Diversity & Inclusion for CUIMC applicants nominated by division chief.
Special Education/Service Plaque (2019) awarded by the International Society for Pediatric Mechanical Cardiopulmonary Support (ISPMCS) in appreciation for valued participation, continued support, and generous donation of time as co-chair of the Scientific and Planning Committees of the 15th International Conference on Pediatric Mechanical Circulatory Support Systems and Pediatric Cardiopulmonary Perfusion, NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY USA
Women in Cardiology, Trainee Award for Excellence, Sponsored by the American Heart Association (2009)
Academic Excellence Award, Maria Fareri Children’s Hospital, Westchester Medical Center, Valhalla, NY (2007)
Research
Selected Publications
- Wittlieb-Weber CA, Villa CR, Conway J, Bock MJ, Gambetta KE, Johnson JN, Lal AK, Schumacher KR, Law SP, Deshpande SR, West SC, Friedland-Little JM, Lytrivi ID, McCulloch MA, Butts RJ, Weber DR, Knecht KR. Use of Advanced Heart Failure Therapies in Duchenne Muscular Dystrophy. Prog Pediatr Cardiol. Accepted for publication: January, 2019.
- Influenza Myocarditis Treated with Antithymocyte Globulin. Piccininni JA, Richmond ME, Cheung E2, Lee TM, Law SP, Addonizio LJ, Zuckerman WA. Pediatrics. 2018 Nov;142(5). pii: e20180884. doi: 10.1542/peds.2018-0884. Epub 2018 Oct 23.
- Changes in renal function after left ventricular assist device placement in pediatric patients: A Pedimacs analysis. Friedland-Little JM, Hong BJ, Gossett JG, Deshpande SR, Law S, Hollifield KA, Cantor RS, Koehl D, Kindel SJ, Turrentine MW, Davies RR. J Heart Lung Transplant. 2018 Oct;37(10):1218-1225. doi: 10.1016/j.healun.2018.06.016. Epub 2018 Jul 24. PMID: 30293616
- Comparison of Transplant Waitlist Outcomes for Pediatric Candidates Supported by Ventricular Assist Devices Versus Medical Therapy. Law SP, Oron AP, Kemna MS, Albers EL, McMullan DM, Chen JM, Law YM. Pediatr Crit Care Med. 2018 May;19(5):442-450.
- Post-transplant outcomes in pediatric ventricular assist device patients: A PediMACS-Pediatric Heart Transplant Study linkage analysis. Sutcliffe DL, Pruitt E, Cantor RS, Godown J, Lane J, Turrentine MW, Law SP, Lantz JL, Kirklin JK, Bernstein D, Blume ED. J Heart Lung Transplant. 2018 Jun;37(6):715-722. doi: 10.1016/j.healun.2017.12.004. Epub 2017 Dec 13
- Delineating Survival Outcomes in Children less than 10 Kg bridged to Transplant or Recovery with the Berlin heart EXCOR Pediatric Ventricular Assist Device. Conway J, St Louis J, Morales D, Law S, Tjossem C, Humpl T. JACC Heart Fail. 2015 Jan;3(1):70-7
- HLA Molecular Epitope Mismatching and Long Term Graft Loss in Pediatric Heart Recipients. Paul Warner, PhD; Mariska S Kemna, MD; Erin L Albers, MD, MSCI; Sabrina P Law, MD; Noel S Weiss, MD, DrPH; Yuk M Law, MD. J Heart Lung Transplant. 2015 Jul;34(7):950-7. doi: 10.1016/j.healun.2014.12.017. Epub 2014 Dec 24
- Impact of Donor-Recipient Sex-Match on Long Term Survival after Heart Transplantation in Children: An Analysis of 5797 Pediatric Heart Transplants. Mariska Kemna, Erin Albers, MD; Miranda C Bradford, MS; Sabrina Law, MD; Lester Permut, MD; D. Mike McMullan, MD; Yuk Law, MD. An analysis of 5797 Heart Transplants. Pediatr Transplant. 2015 Dec 22. doi: 10.1111/petr.12649.
- Eosinophil Count, Allergies, and Rejection in Pediatric Heart Transplant Recipients. Arbon, K., Albers, E., Kemna, M., Law, S., Law, Y. 2015 Aug;34(8):1103-11. doi: 10.1016/j.healun.2015.03.014. Epub 2015 Mar 27
- Dose Conversion Factor between Cyclosporine and Tacrolimus in Pediatric Heart Transplant Recipients. Eliza Notaro, Lisa Brown, Erin Albers, Sabrina Law, Mariska Kemna. J Heart Lung Transplant. 2014 Jul;33(7):766-8.
- Diffuse Rhabdomyomatosis Presenting as Infantile Hypertrophic Cardiomyopathy. Sabrina Law, Terrence Chun, Raj Kapur. J Heart Lung Transplant. 2014 Apr;33(4):452-4.
- Hospital Charges for Pediatric Heart Transplant Hospitalizations in the United States from 1997 to 2006. Sabrina P. Law, MD, Jeffrey J. Kim, MD, Jamie A. Decker, MD, Jack F. Price, MD, Antonio G. Cabrera, MD, Daniel E. Graves, PhD, David L. S. Morales, MD, Jeffrey S. Heinle, MD, Susan W. Denfield, MD, William J. Dreyer, MD, and Joseph W. Rossano, MD. J Heart Lung Transplant 2012;31:485-91
- A newborn with cardiomegaly. Upadhyay S, Law S, Kholwadwalla D. J Emerg Trauma Shock. 2010 Jul;3(3):298. doi: 10.4103/0974-2700.66541.